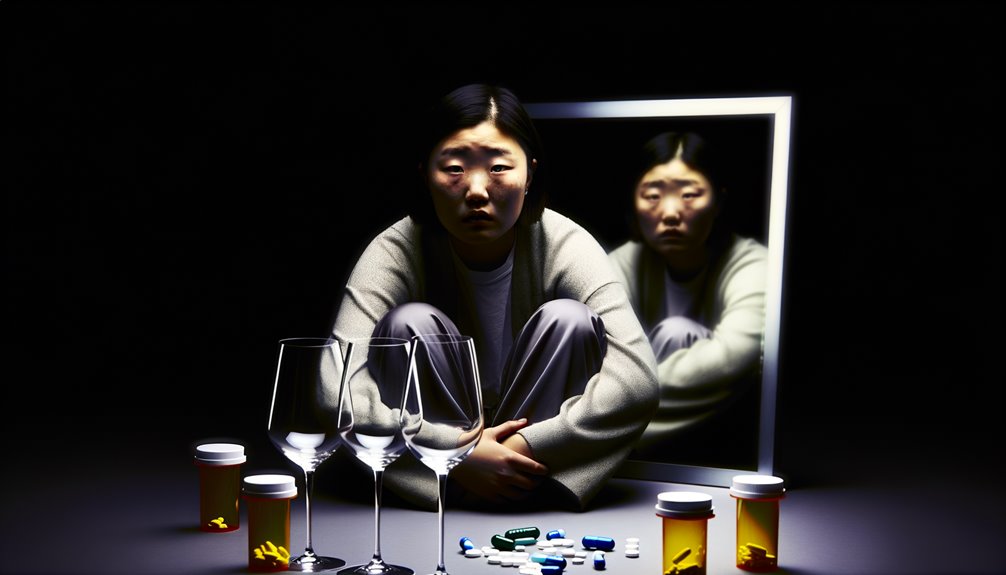
You’re aware that mental health and addiction share a complex, bidirectional relationship. Each condition can worsen the other, creating a challenging cycle of symptoms. Emotional regulation difficulties often lead individuals to self-medicate with substances, while addiction can exacerbate mental health struggles. Neurobiological factors, such as neurotransmitter imbalances, further complicate this interplay. Understanding this intricate connection is essential for effective treatment, and you might wonder how integrated approaches could enhance recovery.
The Bidirectional Relationship Between Mental Health and Addiction
Understanding the bidirectional relationship between mental health and addiction is essential for effective diagnosis and treatment. You’ll often find that co occurring disorders require a dual diagnosis approach to address both mental health and substance use issues concurrently.
Emotional regulation difficulties can exacerbate addictive behaviors, creating challenging behavioral patterns that need specialized treatment modalities. It’s important to bolster psychological resilience, enabling individuals to cope better with life’s stressors without relying on substances.
Reducing stigma is significant in encouraging individuals to seek help and engage with support systems. By understanding this intricate relationship, you can tailor interventions that address both conditions, ensuring thorough care.
Common Risk Factors Contributing to Both Conditions
You should recognize that genetic predisposition plays a significant role in both mental health disorders and addiction, as studies consistently show a hereditary component in these conditions.
Environmental influences, such as exposure to substances or familial dysfunction, further compound this risk by shaping behavioral patterns and stress responses.
Additionally, stress and trauma have been identified as critical factors, often acting as catalysts that exacerbate both mental health issues and addictive behaviors.
Genetic Predisposition Factors
While the complexities of mental health disorders and addiction are influenced by various factors, genetic predisposition plays a vital role in both. You might’ve noticed how certain conditions run in families. This isn’t just coincidence; it’s scientifically backed by genetic markers and familial patterns.
Understanding these can help in diagnosing and predicting vulnerabilities.
Here’s how it might affect you:
- Inherited Traits: Your parents’ genetic makeup could mean you’re more susceptible.
- Shared Genetic Markers: Both conditions can be linked to specific genes.
- Familial Patterns: Having relatives with mental health or addiction issues increases your risk.
- Early Symptoms: You might notice signs earlier due to inherited predispositions.
Recognizing these factors is essential in addressing potential challenges proactively.
Environmental Influences Impact
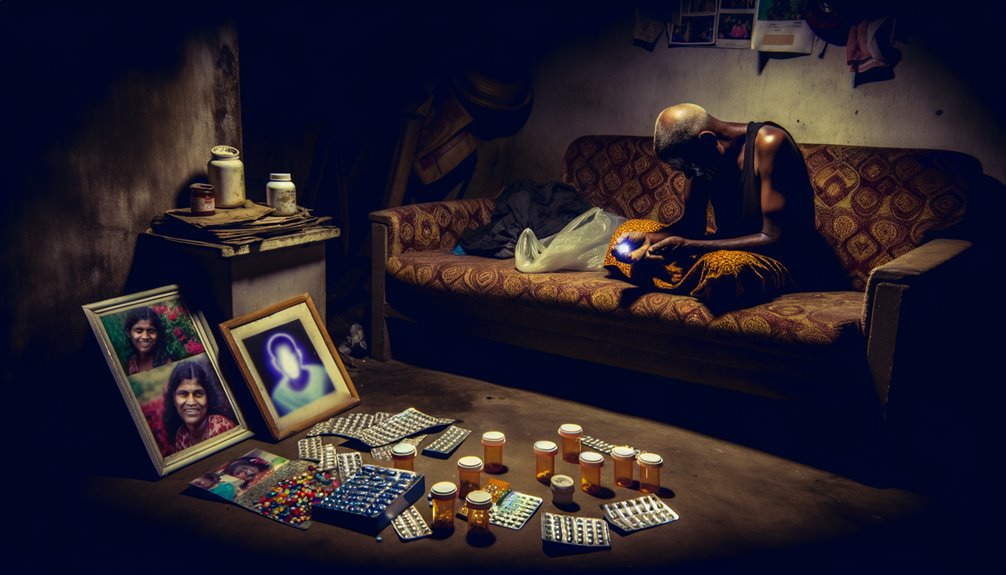
Despite the importance of genetic factors, environmental influences greatly impact the development of mental health disorders and addiction. You should consider how community support or lack thereof affects individuals. A strong support network helps mitigate risks, while isolation can exacerbate them.
Lifestyle choices, influenced by socioeconomic status and cultural norms, play a vital role. Limited educational access often correlates with higher addiction rates and mental health issues. Family dynamics and peer influence shape behaviors and coping mechanisms. Dysfunctional family environments and negative peer pressure increase vulnerability.
Additionally, neighborhood safety impacts mental health; unsafe environments can heighten anxiety and stress, contributing to substance misuse. Recognizing these factors aids in diagnosing and tailoring interventions to address both mental health and addiction effectively.
Stress and Trauma Links
Stress and trauma are vital risk factors intricately linked to the development of both mental health disorders and addiction. Understanding this connection helps in addressing underlying issues through effective therapeutic interventions.
Consider these key elements:
- Stress Management: Without proper coping strategies, stress can spiral into chronic mental health issues.
- Trauma Recovery: Unresolved trauma impacts emotional regulation, often leading to self-medication through substance use.
- Resilience Building: Strengthening resilience through mindfulness practices is essential in mitigating the impact of stress and trauma.
- Support Systems: Having reliable support systems can greatly aid in recovery and prevent relapse.
Evidence-based approaches emphasize resilience, emotional regulation, and mindfulness.
These strategies are integral in promoting healing and preventing the progression of co-occurring disorders.
The Role of Trauma in Mental Health and Substance Use Disorders
You need to recognize how trauma fundamentally alters brain function, often leading to maladaptive coping mechanisms like substance abuse.
Evidence shows that trauma can disrupt neural pathways, increasing vulnerability to both mental health disorders and addiction.
It’s essential to integrate trauma-informed care into recovery strategies to promote effective healing and sustainable recovery.
Trauma’s Impact on Brain
When trauma occurs, it can profoundly alter the brain’s architecture, leading to significant implications for mental health and susceptibility to substance use disorders.
Trauma responses can disrupt brain development, affecting emotional regulation and memory formation. Childhood adversity often triggers neuroplastic changes, influencing long-term effects on mental health. Elevated stress hormones hinder coping strategies and exacerbate vulnerability to addiction.
Consider these profound impacts:
- Emotional regulation disruptions: Trauma skews your ability to manage emotions effectively.
- Memory formation issues: Stress hormones interfere with your brain’s capacity to process and store memories.
- Resilience factors diminished: Childhood adversity reduces your brain’s natural resilience, making recovery harder.
- Long-term susceptibility: Neuroplastic changes can lead to enduring vulnerability to mental health and substance use challenges.
Understanding these changes is essential for effective intervention.
Coping Mechanisms and Abuse
Although trauma profoundly impacts mental health, it’s the coping mechanisms that often dictate the trajectory toward or away from substance abuse. When faced with trauma, you might develop maladaptive coping strategies, such as alcohol or drug use, which can escalate into substance abuse disorders.
Clinical evidence shows that these maladaptive strategies often arise from an attempt to self-medicate emotional pain or distress. Conversely, adopting adaptive coping strategies, like seeking therapy, engaging in physical activity, or practicing mindfulness, can mitigate the risk of substance abuse.
Diagnostic approaches emphasize identifying your specific coping mechanisms to tailor interventions effectively. By understanding and modifying these strategies, you can shift from potential substance dependency to healthier mental health pathways, reducing the likelihood of addiction.
Recovery and Healing Pathways
Understanding the intricate relationship between trauma and substance use disorders can illuminate the pathways to recovery and healing. Trauma often plays a significant role in these disorders, and addressing it is essential for effective treatment.
Employing a diagnostic approach, consider these evidence-based strategies:
- Mindfulness Practices: Cultivate awareness and reduce stress, providing a foundation for healing.
- Holistic Therapies: Integrate practices like yoga and acupuncture to foster physical and emotional well-being.
- Support Systems: Strengthen your recovery journey by connecting with family, friends, and mental health professionals.
- Peer Recovery: Engage with others who’ve walked similar paths for shared experiences and encouragement.
These pathways, grounded in clinical expertise, offer you a thorough route to overcoming trauma-related challenges.
How Neurobiology Links Mental Health and Addiction
Neurobiology plays a pivotal role in linking mental health and addiction, shedding light on how these conditions often coexist. When you examine the brain’s complex systems, you discover that neurotransmitter imbalances can greatly impact both mental health disorders and addiction. Serotonin and dopamine, critical neurotransmitters, influence mood regulation and reward pathways. An imbalance in these chemicals can disrupt brain circuitry, leading to mood disorders or addictive behaviors.
Furthermore, brain imaging studies reveal that changes in brain circuitry, particularly in the prefrontal cortex and limbic system, can alter decision-making and impulse control. This makes you more susceptible to addiction’s grip.
The Impact of Social and Environmental Factors
While neurobiological factors illuminate the intricate relationship between mental health and addiction, it’s equally important to contemplate the powerful role of social and environmental influences.
You’re not isolated in your experience; the community around you can greatly shape your mental health journey. Lack of community support may exacerbate feelings of isolation, increasing vulnerability to addiction.
Environmental stressors, such as poverty or exposure to violence, can trigger or worsen mental health disorders.
Consider these impactful elements:
- Social Isolation – It intensifies feelings of loneliness, leading to substance misuse.
- Community Support – Strong networks can foster resilience and recovery.
- Environmental Stressors – Chronic stress can destabilize mental health.
- Traumatic Experiences – They can leave lasting scars, complicating recovery efforts.
Each factor requires careful evaluation in a thorough diagnostic approach.
Integrated Approaches to Treatment and Recovery
Although the relationship between mental health and addiction is complex, integrated approaches to treatment and recovery offer a promising path forward.
You can benefit from personalized treatment plans that encompass holistic therapies, which address both mental health and substance use disorders. Integrated care combines medical, psychological, and social interventions, ensuring you’re treated as a whole person.
Mindfulness practices, such as meditation, enhance self-awareness and emotional regulation, essential for recovery. Community support plays an important role, connecting you with resources and fostering a network of encouragement.
Engaging in peer recovery groups provides shared experiences and mutual understanding, reinforcing your journey. Evidence shows that these strategies improve outcomes, helping you achieve sustained recovery and well-being through a thorough, coordinated approach.
Strategies for Prevention and Early Intervention
To effectively address the mental health and addiction connection, implementing strategies for prevention and early intervention is essential.
You can play a vital role in reducing risks by engaging in community outreach and promoting educational programs. Encourage support networks and early screening to identify issues before they escalate.
Consider these evidence-based strategies:
- Lifestyle Changes: Encourage healthier choices to reduce vulnerability to addiction and mental health disorders.
- Holistic Therapies: Integrate approaches like mindfulness and exercise to foster overall well-being.
- Awareness Campaigns: Raise public consciousness about the signs and symptoms of mental health issues.
- Peer Support: Foster environments where individuals can share experiences and offer mutual encouragement.
Frequently Asked Questions
What Are Some Common Misconceptions About Mental Health and Addiction?
You might believe mental health and addiction issues are just personal failings, but that’s a misconception.
These are complex conditions requiring professional diagnosis and treatment. Stigma reduction is essential to understanding that they’re not just about willpower.
Treatment accessibility increases when you acknowledge their biological and psychological components. By relying on evidence-based approaches, you can see that recovery involves extensive care, not just a single solution or quick fix.
How Can Family Support Influence Recovery From Addiction?
Family support plays a critical role in addiction recovery. You can improve outcomes through strong support systems, as they provide emotional stability and accountability.
Positive family dynamics foster an environment where you’re encouraged to adhere to recovery plans. Clinically, evidence shows that cohesive families enhance resilience and reduce relapse rates.
Are There Specific Signs Indicating a Dual Diagnosis?
When identifying a dual diagnosis, you’ll notice symptom overlap, such as mood swings or withdrawal signs, complicating a clear diagnosis.
Treatment challenges arise due to the intertwined nature of mental health and addiction, making it essential to adopt an evidence-based, diagnostic approach.
Look for persistent patterns in behavior and mental state fluctuations.
Thorough assessments and personalized treatment plans are critical to effectively addressing both conditions and promoting recovery.
What Role Does Diet Play in Managing Mental Health and Addiction?
When managing mental health and addiction, your diet plays a vital role. Nutritional balance directly influences emotional well-being, as deficiencies can exacerbate symptoms.
Consuming a variety of nutrients supports neurotransmitter production, stabilizing mood and reducing cravings. Evidence suggests that omega-3 fatty acids, vitamins, and minerals are essential for this balance.
Clinically, adopting a diet rich in whole foods can be a diagnostic approach to improving mental health outcomes and supporting recovery from addiction.
How Do Cultural Beliefs Affect Treatment Approaches for Addiction?
Cultural beliefs heavily influence how you perceive addiction treatment. Cultural stigma can deter you from seeking help, affecting treatment accessibility.
You might encounter barriers when cultural norms clash with standard treatment methods. An evidence-based, diagnostic approach considers these factors, ensuring personalized care.
Understanding your cultural background allows clinicians to tailor interventions, improving outcomes. Addressing cultural biases and stigma is essential in making addiction treatment more accessible and effective for everyone.